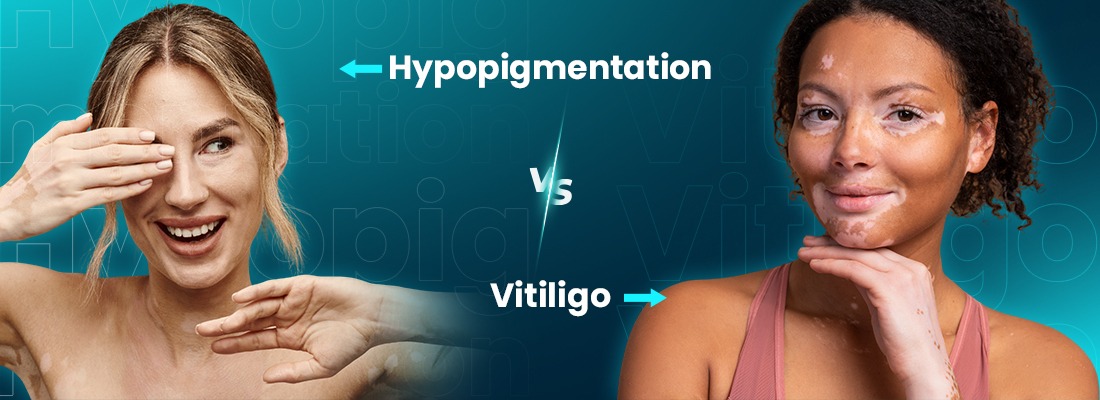
Skin color plays a significant role in how we perceive ourselves, so changes in pigmentation can be both confusing and emotionally challenging. Two commonly misunderstood conditions are hypopigmentation and vitiligo. While they may appear similar at first glance, they are very different in terms of causes, progression, and treatment. Understanding hypopigmentation vs vitiligo is essential for accurate diagnosis, effective care, and peace of mind.
In this blog, we’ll explore the differences between hypopigmentation vs vitiligo, discuss post inflammatory hypopigmentation vs vitiligo, answer common questions like what is the opposite of vitiligo, and connect these insights with ongoing advances in clinical research in dermatology.
What is Hypopigmentation?
Hypopigmentation refers to a partial loss of skin color due to reduced melanin production. Unlike vitiligo, melanin is still present just in lower amounts. This condition often appears as lighter patches that blend gradually into the surrounding skin. Hypopigmentation can occur due to:
- Skin injuries, burns, or trauma
- Inflammatory skin conditions such as eczema or psoriasis
- Fungal or bacterial infections
- Certain medications or medical treatments
Because melanocytes (the pigment-producing cells) are still alive, hypopigmentation is often temporary and may be resolved over time, especially once the underlying cause is treated.
What is Vitiligo?
Vitiligo is a chronic autoimmune condition in which the immune system attacks and destroys melanocytes, as a result, the affected skin loses pigment entirely, leading to well-defined white patches. Vitiligo can affect:
- Skin
- Hair (causing premature whitening)
- Mucous membranes
There are different forms of vitiligo, most notably segmental and non-segmental vitiligo, each with distinct patterns and progression. Understanding these subtypes is critical, which is why many patients explore resources like Understanding the Difference: Non-Segmental vs. Segmental Vitiligo or participate in non-segmental vitiligo clinical trials to access emerging therapies.
Hypopigmentation vs Vitiligo: Key Differences
When comparing hypopigmentation vs vitiligo, several important distinctions stand out:
1. Cause:
- Hypopigmentation: Reduced melanin production due to injury, inflammation, or infection
- Vitiligo: Autoimmune destruction of melanocytes
2. Pigment Loss:
- Hypopigmentation: Partial pigment loss
- Vitiligo: Complete pigment loss
3. Patch Appearance:
- Hypopigmentation: Lightened patches with softer borders
- Vitiligo: Milky-white patches with sharp, defined edges
4. Progression:
- Hypopigmentation: Often improves or resolves
- Vitiligo: Chronic and may spread over time
These differences between hypopigmentation vs vitiligo are crucial for dermatologists when determining diagnosis and treatment plans.
Post-inflammatory Hypopigmentation vs Vitiligo
One of the most common areas of confusion is post-inflammatory hypopigmentation vs vitiligo. Post-inflammatory hypopigmentation occurs after the skin heals from inflammation or injury. Conditions such as acne, dermatitis, or laser treatments can temporarily disrupt melanin production. The result is lighter patches that gradually regain color.
Vitiligo, on the other hand:
- Is not triggered by healing or injury alone
- Does not resolve on its own
- Often requires long-term management
If the skin color begins to return over weeks or months, it is more likely post-inflammatory hypopigmentation rather than vitiligo.
What is the Opposite of Vitiligo?
A common question patients ask is: what is the opposite of vitiligo?
While vitiligo causes loss of pigment, its opposite would be hyperpigmentation, a condition where excess melanin leads to darker patches of skin. Examples include melasma, post-inflammatory hyperpigmentation, and sun-induced dark spots.
Interestingly, some individuals experience both hypo- and hyperpigmented conditions at different times, emphasizing the complexity of pigment regulation.
Is Vitiligo Genetic or Hereditary?
Many people worry about passing vitiligo to their children. Research shows that vitiligo has a genetic component, but it is not directly inherited in a predictable pattern. Having a family member with vitiligo increases risk slightly, but environmental and immune factors also play a significant role.
Is Vitiligo Considered a Disability?
Another important concern is whether vitiligo qualifies as a disability. Medically, vitiligo does not impair physical functioning. However, its psychological and social impact can be significant, particularly in cultures where appearance plays a strong role in social acceptance. In some regions and circumstances, vitiligo may be recognized under disability protections due to its emotional and mental health effects.
Vitiligo vs Other Pigment Disorders
Vitiligo is often confused with other conditions such as leucoderma or albinism. While these disorders all affect pigmentation, they differ greatly in cause and presentation.
- Albinism is a genetic condition present from birth and affects the entire body, including eyes and hair, as explored in Albinism vs Vitiligo: Key Differences, Causes, and Symptoms.
- Leucoderma is a broader term for white patches on the skin and may include vitiligo as one of its causes.
The Role of Research and Clinical Trials
Advancements in treatment are being driven by ongoing clinical research in dermatology. From topical therapies to immunomodulators and regenerative approaches, research is transforming how vitiligo is managed. Many patients with widespread or progressive disease consider enrolling in non-segmental vitiligo clinical trials, which offer access to innovative therapies not yet widely available.
Final Thoughts
While hypopigmentation and vitiligo may look similar, they are fundamentally different conditions with distinct causes, outcomes, and management strategies. Understanding hypopigmentation vs vitiligo, including post inflammatory hypopigmentation vs vitiligo and related concerns like what is the opposite of vitiligo empowers patients to seek accurate diagnoses and informed care.
If you notice changes in your skin color, consulting a dermatologist is essential. With ongoing research, growing awareness, and expanding treatment options, there is more hope than ever for individuals navigating pigment-related skin conditions.