Updated on July 20, 2022
Overview
Prurigo Nodularis (PN) is a chronic inflammatory skin disease that is characterized by a highly itchy, symmetrically distributed rash throughout the arms, legs, upper back, and/or abdomen.
The itch brought on by PN is so severe that it frequently interferes with sleep and mental health.
It is a chronic inflammatory skin condition marked by itchy nodules. Unmistakable excoriated nodular, hyperpigmented/purpuric lesions with crusted or scaly surfaces are symptoms of this condition that are further exacerbated by persistent scratching. Prurigo nodularis treatment can help reduce the severity of the symptoms however, treatment is a requirement as PN lesions very rarely disappear spontaneously.
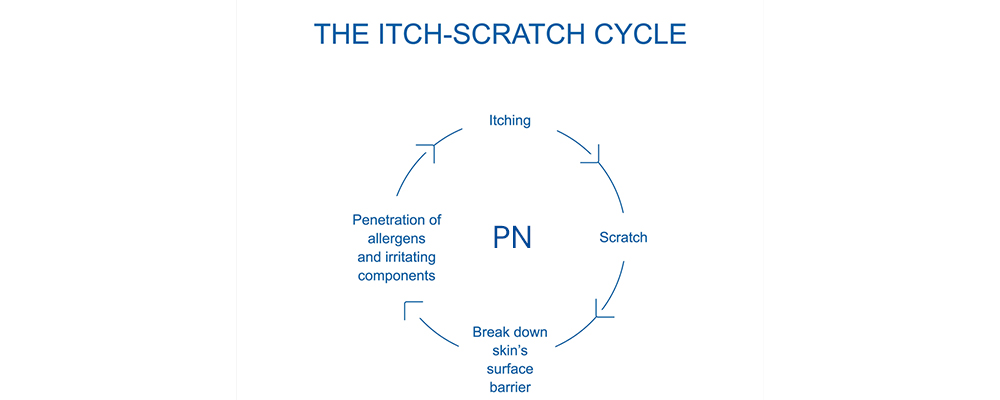
The itch-scratch cycle appears to be triggered by immunological and neurological abnormalities, despite the fact that the illness’s true cause is unknown. Throughout this blog, we’ll be covering as much information about the condition, its causes, its possible treatment, Prurigo nodularis foods to avoid, and so on.
What is Prurigo Nodularis?
Prurigo Nodularis (PN) is a skin condition that results in the development of hard, itchy lumps (called nodules) on the skin. Itching (pruritus) can be so bad that people scratch themselves until they bleed or feel pain. Lesions can spread if they are scratched. There is no known cause for PN. Although it is well known that scratching leads to the development of additional nodules. The disease is diagnosed by looking for symptoms like extremely scratchy skin that develops nodules. Occasionally, a skin biopsy is performed to confirm the diagnosis and this helps your physician come up with a Prurigo Nodularis treatment plan for you.
Who gets Prurigo Nodularis?
Although Nodular Prurigo can strike anyone, it most frequently affects people in their 20s to 60s. Both genders are equally affected. People with other pruritic skin conditions, such as atopic dermatitis (eczema), cutaneous T-cell lymphoma, lichen planus, xerosis cutis, keratoacanthomas, and bullous pemphigoid, are most frequently found to have PN.
Usually, PN can be mistaken for other skin diseases and can co-occur with some of them because of this and symptoms overlap with other conditions that cause severe, chronic pruritus.
What is the Etiology of Prurigo Nodularis?
Despite the fact that Prurigo Nodularis seems to be very common, particularly in people with associated or precipitating diseases, its incidence in the general population has not yet been investigated. Prurigo nodularis treatment can help different people suffering from this condition. It is most common in people who:
- Are African-Americans, usually between the ages of 51 and 65. And if they frequently suffer from Atopic Dermatitis flares, the chances of developing Prurigo Nodualris increase.
- Have ongoing chronic illnesses.
- Have long-term conditions linked to a higher risk of Prurigo Nodularis development including diabetes, end-stage renal disease, contact dermatitis, and atopic dermatitis.
- Have the Hepatitis C virus or their HIV has not been treated.
- Have depression and anxiety due to Hodgkin’s and non-lymphoma Hodgkin’s depression, and a few other mental health problems.
It’s important to remember that Prurigo Nodularis can affect anyone at any age, even though some people are more inclined to the condition than others.
What Characteristics of Nodular Prurigo are Clinical?
Each Prurigo Nodule is a solid, 1-3 cm in diameter lump that frequently has a raised warty surface. Smaller red itchy bumps may initially appear as the early lesion. Scratched lesions may be covered by scaling and crusting. Lesions that are older than the surrounding skin may be paler or darker. Frequently dry skin can be found between the nodules. The itch is extremely strong, frequently lasting for hours on end, which causes vigorous scratching and occasionally secondary infection. Prurigo nodularis treatment is usually aimed at treating these symptoms or reducing them.
Nodular prurigo lesions are typically numerous and grouped, but their number can range from 2-200. The distribution of nodular prurigo is symmetrical. Typically, they begin on the lower arms and legs and get worse on the outside. Additionally impacted areas include the palms, face, and trunk. On occasion, the nape region is where prurigo nodules are most noticeable (neck, shoulders, and upper arms).
What causes Prurigo Nodularis?
In most cases, there is a clear cause. An inherited disease like asthma, eczema, hay fever, or hives is present in 50% of Prurigo Nodularis cases.
- Prurigo nodularis can appear in stasis eczematous dermatitis, a common type of dermatitis of the lower legs that is linked to blood pooling or “stasis” in the veins. Additionally, it can be seen in people who have lichen simplex, insect bite reactions, and nummular eczema, a common form of eczema with distinct, coin-shaped sores.
- A metabolic or biochemical factor causes itching in 30% of Prurigo Nodularis cases. This may include, insufficient nutrition, an abnormal liver, or Uraemia.
- Thyroid disease, neurological disease (stroke), hypercalcemia (high blood calcium levels), and lymphoma are less frequent causes.
- Reduced iron absorption is the most common sign of nutritional deficiency in the blood. The most common cause of additional loss is diet-related (i.e. underlying iron deficiency due to eating habits of females with excessive menstrual iron loss). Gluten hypersensitivity can lead to iron malabsorption (compromised absorption of iron in the gut), though this happens most frequently after bowel surgery).
- The remaining 20% of those affected by Prurigo Nodularis are affected by psychological conditions like psychosis, anxiety, and depression.
Those who suffer from Prurigo Nodularis frequently have all three underlying causes (atopic, psychological, and nutritional). The “lonely, malnourished depressive” is a condition in which atopic dermatitis is both precipitated and sustained by acute depression. For the Prurigo Nodularis treatment, not just the itchy nodules need to be treated; also the tendency toward eczema, depression, and diet.
What Prurigo Nodularis Symptoms are Present?
A tiny, red, itchy bump could be the first sign of PN. The pruritic nodules can appear anywhere on your body where you scratch, but they typically develop on your arms or legs.
The nodules could cause excruciating itching. The bumps can have a variety of colors, from flesh tones to pink, brown, or black scabby warty-looking bumps that are hard, crusty, and scaly. Some people with PN experience temperature changes, burning, and stinging in their bumps. They might disappear if the person refrains from scratching the nodules. They might sometimes leave scars. People with this condition usually receive Prurigo Nodularis treatment plans that are more inclined toward symptomatic treatment.
Here are a few additional signs that people with Prurigo Nodularis encounter:
- Patients who have it typically are middle-aged or older, though it can also affect children.
- Long-standing pruritus in the affected areas is a persistent complaint from the patient.
- There are distinct painful areas that eventually give rise to symmetrically distributed pigmented nodular lesions.
- Nodules typically have a fixed size and do not disintegrate on their own.
- The quantity of nodules increases over time.
- One of the linked disorders (see “Associated diseases” below) might run in the family.
- Itching and worry about the cause of the lesion are fairly typical.
In contrast to 25% of the general population, up to 80% of people with Prurigo Nodularis have a personal or family history of atopic dermatitis, asthma, or hay fever.
Diet and Prurigo Nodularis:
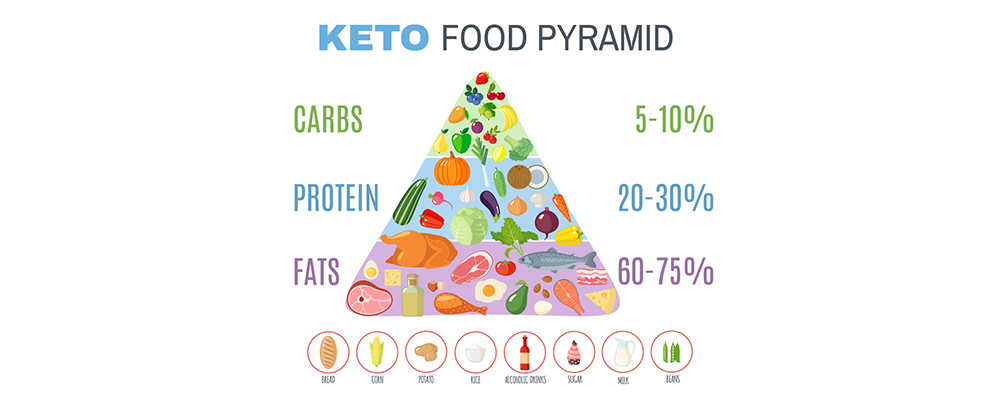
PN is sometimes called a “keto rash” because it is associated with people who follow strict diets, particularly a ketogenic diet. A ketogenic (keto) diet entails eating a lot of fat-based foods and limiting your carbohydrate intake. This eating regimen induces the metabolic state of ketosis (the body uses stored fat for energy). Prurigo nodularis foods to avoid include fat-based foods.
People frequently adhere to the diet in order to lose or maintain their weight because it is effective at doing so. However, some people also use it to lower their risk of diseases like diabetes, hypertension, and heart disease, which are linked to obesity.
According to researchers, the gut microbiome may be involved in this association (the microorganisms in your digestive tract). As a result, PN may result from a gut microbiome imbalance that affects a person’s immune system.
Prurigo nodularis Foods to Avoid:
Your doctor might suggest stopping the ketogenic diet if Prurigo Nodularis is connected to ketosis. Typically, this means maintaining a balanced diet while limiting your intake of refined foods and foods that cause inflammation, such as:
- Red meat
- Processed food with high levels of additives and preservatives
- Trans fat
- Fried food
- Refined sugars and flour
As with any form of the treatment plan including Prurigo Nodularis treatment, altering your diet when directed to do so by a qualified healthcare professional such as a nutritionist or dietician can have a positive impact on the treatment and your quality of life.
Prurigo Nodularis Foods to Consume:
Incorporating nutritious foods is crucial in reversing Prurigo Nodularis brought on by ketosis, in addition to Prurigo Nodularis foods to avoid which is unhealthy fats. In particular, when you have PN, reintroducing carbohydrates is essential for changing your diet.
Your gut microbiome can be rebalanced by concentrating on complex carbohydrates that are high in fiber and primarily made from plant sources. Complex carbohydrates allow blood sugar to rise more gradually because they digest more slowly than simple carbohydrates (such as sweets and refined sugar).
Include the following in your diet to add more nutrient-dense carbs:
- Veggies high in starch (potatoes, sweet potatoes, corn, beets, squash)
- Sour fruits (bananas, dates)
- Legumes (lentils, beans)
- Entire grains (whole-wheat bread, rolled oats, quinoa)
- Increasing your intake of anti-inflammatory foods may also help with healing since PN is an inflammatory condition.
Foods that reduce inflammation include:
- Spices (basil, cinnamon, cumin, curry, ginger, turmeric)
- Wholesome fats (salmon, herring, flax, chia seeds)
- Veggies and fruits
- Dark chocolate
- Green tea
How is Prurigo Nodularis Treated?
The most common option for Prurigo Nodularis treatment involves the use of topical or intralesional steroids. In more severe cases or patients who are resistant to treatment, phototherapy or systemic immunosuppressives are frequently necessary.
Localized Treatment:
Here are a few instances:
- Emollients are frequently applied to itchy skin to cool and soothe it; menthol may be added to increase the soothing effect.
- In addition to being administered intravenously or orally, steroids can also be applied topically or under occlusive dressings to lessen inflammation and pruritus and soften smooth nodules. The answer is frequently unpredictable.
- Injections of intraocular steroids are occasionally used.
- It has been demonstrated that phenol and local anesthetic lotions are helpful.
- Sometimes, coal tar cream is applied in place of steroids.
- In some circumstances, calcipotriol ointment is more efficient than topical steroids.
- Capsaicin cream causes burning and irritation but may also eventually stop itching. It must be applied four to six times daily.
- Cryotherapy with liquid nitrogen can reduce nodules and stop itching.
- By using a pulsed dye laser, the vascularity of specific lesions can be decreased.
Systemic Prurigo Nodularis Treatment:
Here are a few medications that may help:
- Antihistamines may occasionally be able to reduce itching.
- Systemic corticosteroids have a wildly inconsistent response.
- Cyclosporin, methotrexate, and azathioprine have all been discovered to be useful in some circumstances.
- In severe cases, thalidomide has been shown to be extremely helpful; however, it is linked to teratogenicity and peripheral neuropathy.
- Naltrexone is an opiate-receptor antagonist that has been used as Prurigo Nodularis treatment that has shown some promise in the treatment of itch.
- Systemic retinoids, like acitretin, may reduce the nodules and soothe irritation.
- Although there are risks associated with prolonged UV exposure, psoralen combined with ultraviolet A (PUVA) treatment may be advantageous.
- In severe, refractory cases, there is anecdotal evidence of a positive response to the immunomodulatory macrolide roxithromycin, either by itself or in combination with the anti-fibroblast medication tranilast.
- Effective use of gabapentin has been made. It has the capacity to sedate people, though.
Itch-Scratch Cycle associated with Prurigo Nodularis:
The “Itch-Scratch Cycle” in people with Prurigo Nodularis may be greatly influenced by psychological distress and hopelessness, which can lead to a pruritic feeling and scratching that perpetuates the illness. According to one study, people with Prurigo Nodularis frequently experience anxiety and depression. The following are some methods for treating this condition:
- Psychological counseling (CBT): Patients must be ready to accept a psychological model of their problem in order to respond, and there is little evidence of efficacy.
- Utilizing Habit Reversal Therapy, which was initially developed to treat tics. It has been observed that it can break the “Itch-Scratch Cycle”.
Although the use of Anxiolytic drugs may be advantageous, addiction is a possibility. Antidepressants like Amitriptyline and Doxepin may also be advantageous.
Takeaway:
Prurigo nodularis is an extremely itchy skin condition that can be incapacitating. Although the exact cause is unknown, it is known to be linked to a number of other conditions.
Although there are many Prurigo Nodularis treatment options available, it might take some time to successfully manage your PN. You’ll probably benefit from a mix of topical, pharmaceutical, and healthy lifestyle changes including what to consume and Prurigo Nodularis foods to avoid.
The good news is that numerous new medications and potential Prurigo Nodularis treatments are being developed and tested. More specialized, efficient therapies will be developed as researchers gain a better understanding of the PN mechanism.